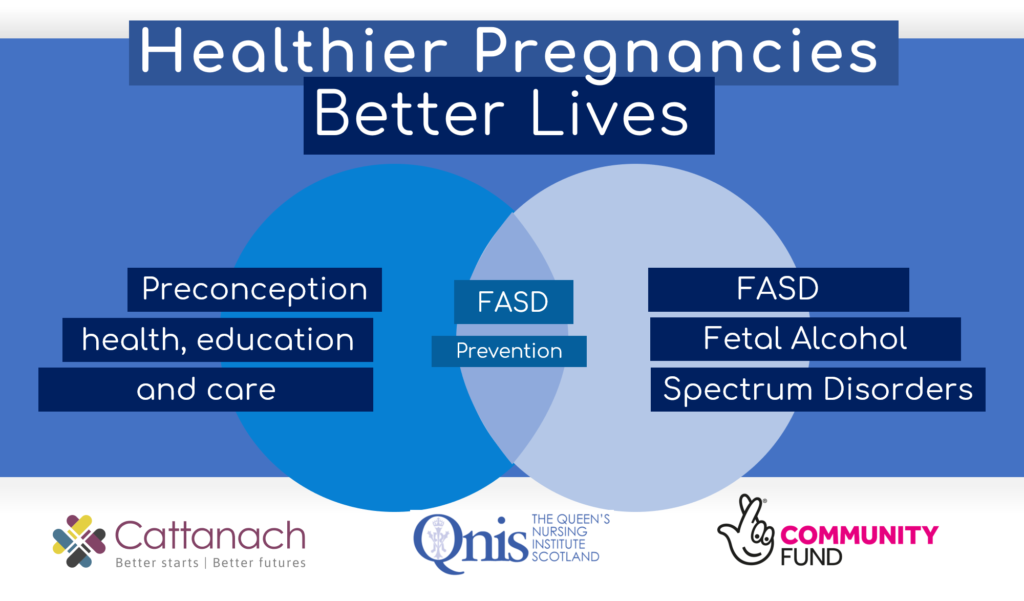
Fetal Alcohol Spectrum Disorders can have a devastating impact on the development of children. It’s estimated up to 172,000 people are affected in Scotland but less than 1% have had a formal diagnosis. To help tackle this the Queen’s Nursing Institute Scotland are campaigning for Healthier Pregnancies, Better Lives. As part of that campaign Joan Gracie, a supervisor for the Family Nurse Partnership with NHS Forth Valley talks here of addressing blind spots in preconception health.
Over the past 30 years as a nurse I’ve worked in a variety of roles in community settings: Health Visitor, Team Leader for School Nursing, and now as a Supervisor for the Family Nurse Partnership. In all these years, I never encountered anyone who had a diagnosis of Fetal Alcohol Spectrum Disorder (FASD). I have often wondered why.
I was recently invited to work with QNIS to help plan a five-year programme that will address Scotland’s longstanding blind spots around both preconception health and FASD. I am looking forward to doing this along with other, like-minded Queen’s Nurses and other colleagues. We want this to lead to greater understanding, meaningful actions and real benefits for individuals, families, communities and Scottish society.
This QNIS programme will develop bespoke Scottish tools, resources and leadership training. These should be catalysts for better preparation for pregnancy; that is, preconception health, education and care. They should also help community nurses and other professionals act upon the need for a better understanding of such life-long conditions as FASD that have pre-natal roots.
We know that the periods of preconception and pregnancy are the earliest and most critical stages at which services can put in place effective interventions to prevent long-term harm to children and families. Community nurses are ideally placed to take positive action in a variety of settings, including School Nursing, Sexual Health Services, Health Visiting, General Practice, Community Midwifery, Looked After Care, Learning Disability Nursing and Drug and Alcohol Services. Because both preconception health and FASD have largely been missing from the professional education and development of nurses and midwives, making our contribution requires increased competence and confidence.
Recently, as I was speaking to a paediatrician in my health board, she said:
“As my mother was being formed in her mother’s womb, a part of me was being formed in my mother’s womb.”
Let’s think about that for a moment and what it means for the responsibility that we have in community health care settings to raise awareness of preconception health and FASD.
FASD is a lifelong, neurodevelopmental condition that is potentially preventable, but so often not prevented. Children, young people and adults display a range of behavioural, physical, emotional and developmental concerns as a result of having been exposed to and affected by alcohol prenatally. This is a hidden or invisible disability, with only around ten percent of those affected displaying any facial features associated with the condition, (small eye openings, a thin upper lip and a smooth philtrum).
The Scottish Government has estimated that up to 172, 000 people are affected by FASD. Less than 1% have ever received a formal diagnosis or appropriate assistance. One Scottish study showed that, between 2010-2015, only 41 children were reported as diagnosed with FASD, Given Scotland’s relationship with alcohol, it is worth reflecting on this very low incidence of diagnosis.
As I learn more about the subject, it is clear that there are multiple reasons for such a low incidence of reporting FASD in Scotland. One is lack of education, so professionals may not consider that prenatal alcohol exposure (PAE) could be a potential cause of developmental delay and behavioural difficulties in children and young people. It is only recently that a standard diagnostic tool and Scottish guidance have become available. Research also shows that children are too often not being referred for appropriate assessment when alcohol use during pregnancy is suspected.
In my own experience, where mothers use drugs, this concern often overshadows discussion about alcohol use. Drug misuse is viewed as uncommon and unacceptable. Drinking is normal and seen as a potential problem only when someone regularly gets drunk.
Some characteristics of FASD are similar to those of ADHD, ASD and other neurodevelopmental conditions. In the past, assessments usually stopped as soon as one satisfactory diagnosis was found. Yet, these conditions often co-exist and are not ‘either/or’ diagnoses. People can be affected, for example, by both ADHD and FASD.
It perhaps feels humane not to ask about drinking during pregnancy when professionals are presented with a child who has developmental delay or learning and behavioural difficulties. This can arise from a desire to protect parents from the knowledge that they may have inadvertently caused harm to their baby. However, we must work together to find better ways of discussing this in a non-shaming manner with parents, so that children will receive a proper diagnosis and bespoke support plans as early as possible.
To explore the myths, realities and practical steps community nurses can take, the new, NES eLearning resource about FASD is an excellent site.
In contemporary Community Nursing, our practice is based on health-creating models, with person-centred care at its core. We work from a strength-based perspective to enable and empower people, providing them with the knowledge to make their own decisions about their health.
Preconception health, education and care offers a wonderful opportunity to put those principles into practice. We can help keep harm from happening while assisting men and women prepare well for pregnancy. As a health visitor, I look back and now see missed opportunities to help parents prepare for the next pregnancy in ways that could have improved the outcome.
As a community nurse and a Queen’s Nurse, I’m excited about this new QNIS programme, Healthier Pregnancies, Better Lives. Preconception health and FASD have been hiding in plain sight for decades. We should open our eyes to the bad news (and the good news) about the long-lasting impacts of what happens before birth, and even before pregnancy. That will help us see the people we care about, and care for, more clearly.
Five years from now, community nurses should no longer be repeating my experience of never encountering anyone with an FASD diagnosis. Knowing what we’re seeing, knowing how to help and knowing how to prevent further harm should become a normal part of what we do.
This blog first appeared on the QNIS website and has been re-published with the kind permission of Joan, QNIS and NHS Forth Valley. For further information or to express an interest in QNIS’ Healthier Pregnancies, Better Lives programme contact jonathan.sher@qunis.org.uk